Organoids, AI, and the FDA’s Move Away from Animal Models
Inside the FDA’s push to replace lab animals with human tissues & algorithms — with scientist Dr. Patrick Creisher.
For nearly a century, animal testing has been a pillar of biomedical research. Since the 1938 Food, Drug, & Cosmetic Act, passed in the wake of the Elixir Sulfanilamide disaster, drug developers in the U.S. have been required to test new compounds on animals, typically two species, before beginning human trials.
But that status quo began to shift in 2022, when the FDA Modernization Act 2.0 eliminated the federal requirement for animal testing in preclinical drug development. A series of regulatory changes, including a major FDA announcement on April 10, 2025, now signals that we are entering a new age where tests on lab animals may no longer be the standard for drug safety.
In this week’s Biotech Blueprint podcast, I spoke with Dr. Patrick Creisher, PharmD, PhD, a scientist who transitioned from using animal models during his doctoral studies to working with human organoids in his postdoctoral research. With firsthand experience on both sides, Patrick offers a unique perspective on what this shift means for science, industry, and ethics.
The FDA’s new roadmap outlines how the agency will reduce or even replace animal testing in the development of monoclonal antibodies and other therapies. The agency is encouraging the use of “New Approach Methodologies” (NAMs): AI-based computational models of toxicity, and cell lines and organoid toxicity testing in a lab setting.
These methods, the FDA argues, are more human-relevant, more scalable, and potentially faster and cheaper. Commissioner Dr. Martin Makary called it a “paradigm shift,” and noted that this change could accelerate cures, reduce drug development costs, and spare thousands of lab animals each year.
But as Patrick and I discussed, replacing animal models is easier said than done. Organoids (miniaturized, lab-grown versions of human organs derived from stem cells) are increasingly seen as promising alternatives. The FDA now encourages their use in drug development, particularly when validated alongside animal models, as part of a broader effort to modernize preclinical testing.
Because they are human-derived, organoids often offer better predictive power than animal models for certain toxicities and disease mechanisms. However, they remain simplified systems: they lack blood vessels and immune cells, and are may not be mature enough to replicate the full complexity of a living organism. They are useful, but not yet a complete substitute and to date, no drug has been approved based solely on organoid data.

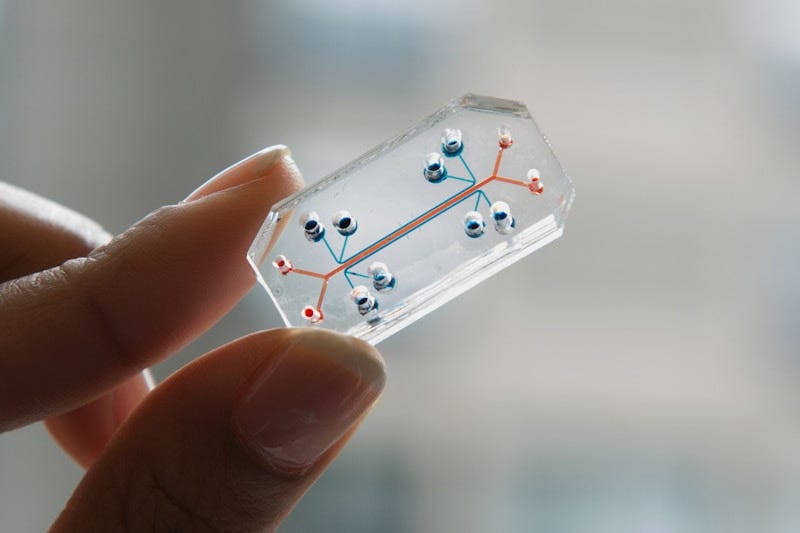
Organs-on-chips, another alternative, simulate specific functions like kidney filtration or cardiac contraction. Companies like Emulate, Mimetas, and TissUse are developing modular systems that link multiple organs to study how drugs are metabolized in the body. But these tools remain technically complex and expensive. And while they offer specificity, they can fall short in capturing systemic responses, such as immune interactions and the full complexity of central nervous system activity.
That brings us to what may become a major force in the future of drug development: artificial intelligence. Companies like Insilico Medicine and VeriSIM Life are pioneering in silico drug development, using AI to design and test compounds before going to the lab. Insilico recently advanced an AI-designed fibrosis drug to human trials with minimal animal testing, while VeriSIM’s BIOiSIM platform builds virtual models of humans and animals to predict pharmacokinetics, toxicity, and efficacy. Their Translational Index, inspired by a credit score, helps rank which compounds and which species are most likely to deliver meaningful results.
These platforms promise major improvements in speed, cost, and ethical footprint. But they’re not without limitations. AI models are only as reliable as the data they’re trained on, and for rare toxicities or less-understood biological responses, data may be scarce. Transparency, rigorous validation, and thoughtful integration with experimental data will be essential.
Following the FDA’s April 10, 2025, announcement to phase out animal testing requirements for certain drugs, Charles River Laboratories, a major supplier of lab animals, saw its stock price dip sharply by about 28%. Patrick and I explored whether companies like Charles River and Jackson Labs will need to adapt or risk becoming less central to the future of drug development. The answer? Likely not yet. Currently, the industry is moving toward a hybrid model where AI, organoids, and organ-on-chip technologies complement, rather than replace, animal studies. Additionally, academic research may continue to rely on animal models longer than the private sector.
Within a few years, we may see formal FDA guidance on submitting organoid or chip-based data for investigational new drugs. In 10+ years, animal testing could become “animal-optional,” reserved only for special cases where no viable alternative exists. The vision is not just scientific but ethical. As AI and tissue engineering mature, we may one day build human avatars that recapitulate immunity, neurobiology, and metabolism, delivering better drugs with fewer animals, fewer risks, and faster timelines.
The question is no longer whether we move away from animal testing, but when and how. If the FDA’s roadmap holds, the future could be not only more humane, but also more scientifically rigorous.
Thanks for reading Biotech Blueprint. If you enjoy the content, please subscribe to support this effort.
Thank you.
DISCLAIMER: This content is for informational purposes only. It should not be taken as legal, tax, investment, financial, or other advice. The views expressed here are my own and do not reflect the opinions of any company or institution.
DISCLOSURE: I have no business relationships with any company mentioned in this article.






Fascinating concept, using these human driven organoids might be more accurate for testing purposes than on animals.
I’m wondering if there is any data on clinical success rates based on the use of organoids at the pre-clinical stage? Too early perhaps?